This page was reviewed under our medical and editorial policy by Toufic Kachaamy, MD, Chief of Medicine, City of Hope Phoenix This page was reviewed on January 17, 2022.
A stool test is a fairly simple, non-invasive colon cancer screening option. There are several types of fecal or stool-based tests available, and each has its share of advantages and disadvantages to consider. Unlike a colonoscopy, these tests don’t require prep work. It’s important to note, however, that if you have a positive result, you will still need a colonoscopy or another test to confirm the findings and remove any precancerous polyps. Colonoscopy, a visual and more detailed exam of the colon, is considered the best option for colorectal cancer screening.
Also known as: Immunochemical fecal occult blood test, iFOBT
Why it’s performed: The fecal immunochemical test (FIT) looks for hidden blood in the stool. This may be an early sign of colon cancer, although not all cancers or polyps bleed. This test only detects blood that comes from your lower intestines, not further up your digestive tract.
Cost: Medicare covers FIT once a year if you’re 50 or older, as do most private insurers.
Pros and cons: It’s easy to do, it takes just a few minutes and no changes to your diet or current medication regimen are needed. Just one stool sample is needed, unlike other stool tests that may require multiple samples.
Also known as: Guaiac test, gFOBT, guaiac smear test
Why it’s performed: The fecal occult blood test (FOBT) looks for hidden or occult blood in the stool. Guaiac is used to coat the FOBT test cards. It creates a chemical reaction with stool if blood is present. This test can’t determine if the blood is from your colon, rectum or other parts of your digestive tract. For this reason, it’s considered less specific than the FIT test.
What happens during the procedure: This test can be performed at home or during a regular appointment as part of a rectal exam. At home, you’ll be asked to:
Unlike FIT, the FOBT test does require some prep.
What the results mean: If there is blood in your stool, it may be coming from the stomach or intestinal tract. There are many potential reasons for this, including colon cancer or colon polyps, but it also may be false-positive. It typically takes roughly one to three days to get results. You’ll likely need a colonoscopy if the FOBT test is positive.
Cost: Medicare covers yearly FOBT if you’re 50 and older, as do most private insurers. Call your carrier to make sure the cost is covered.
Pros and cons: This stool-based test is inexpensive and can be done at home. If it’s done during a rectal exam, however, it may be uncomfortable. It has a high false-positive rate, because it is not specific for human blood and casts a wider net than FIT. You also have to watch your diet before the test and may need to stop taking certain medications for more accurate results.
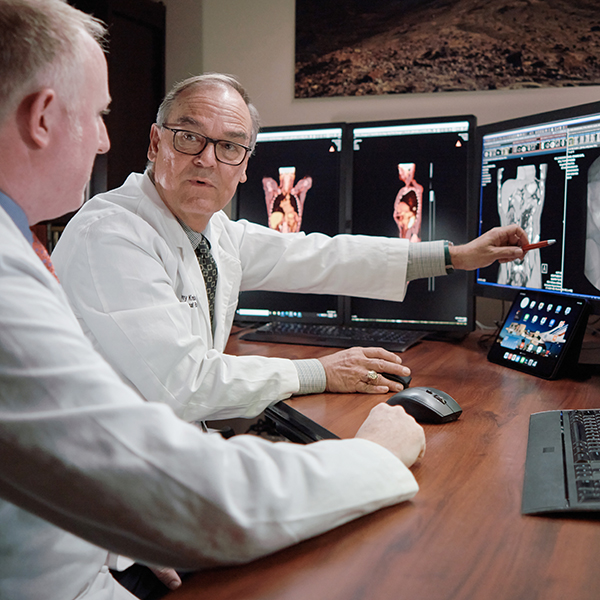
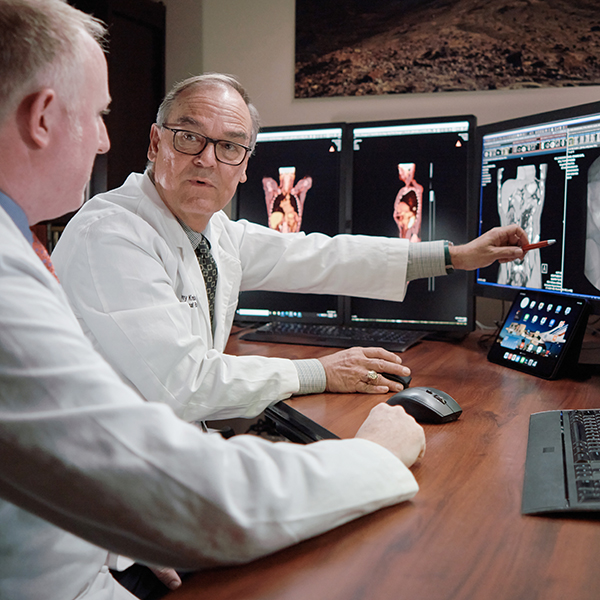
Your multidisciplinary care team will work with you to develop a personalized plan to treat your colorectal cancer in a way that fits your individual needs and goals.
Also known as: Cologuard ®
Why it’s done: Stool DNA testing is a newer type of non-invasive stool-based test to check for colorectal cancer. It looks for certain DNA or genetic changes that may suggest pre-cancerous growths or cancer cells. It should be repeated every three years.
What happens: Your doctor will order a kit that contains everything needed to collect a DNA stool sample. To start:
You don’t have to make any changes to your diet or medication regimen to take this test.
What the results mean: If a stool DNA test finds something abnormal, a colonoscopy may be needed to follow up on the findings. Your doctor should have the results within two weeks from the time that the sample is received at the lab.
Cost: Stool DNA tests are more expensive than other stool-based tests. If it’s not covered by insurance, the cost is around $565.
Pros and cons: There is no prep required, and this test requires only one stool sample. It is believed to be more accurate than the FIT test.
Everyone is different, so it’s important to discuss personal medical history and risk factors with your doctor when deciding which colorectal screening methods are most appropriate for you and how often you should be screened.